A severe case of patient neglect at Princess Margaret Hospital (PMH) has ignited public outrage and raised urgent questions about healthcare standards in The Bahamas’ primary public medical facility. Branyiell Hall, a 28-year-old sickle cell patient and mother, endured an agonizing night lying in soiled bedding without assistance following surgical procedures, according to her family’s account.
The incident occurred in the Female Medical-Surgical Ward East where Hall, weakened and immobilized post-operation, remained completely dependent on nursing staff. Her sister, Branae Russell, reported leaving the hospital after visiting hours concluded, confident that medical professionals would provide adequate overnight care.
Instead, Hall spent approximately twelve hours unattended in urine-soaked conditions, unable to secure assistance despite repeated calls for help. A distressing 57-minute voice message captured the patient’s emotional and physical distress as she described her ordeal of being left unchanged since immediately after surgery.
This case highlights systemic challenges within PMH, which faces a documented shortage of approximately 500 registered nurses according to recent institutional disclosures. While Hall eventually received attention from morning shift staff who administered pain relief and cleaning assistance, the psychological impact of the neglect has been profound.
The family emphasizes this represents not an isolated incident but rather a pattern of concerning care deficiencies, particularly during night shifts when patient vulnerability increases. Russell’s social media appeal for ministerial intervention has garnered significant public support, with hundreds sharing her post demanding accountability and improved patient dignity standards.
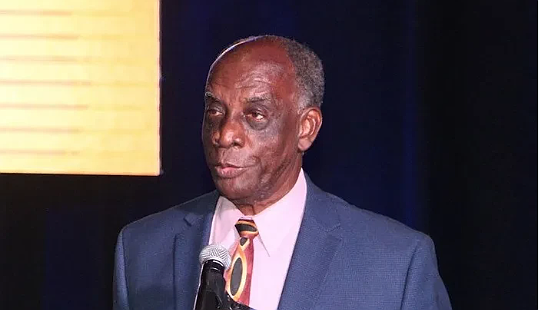
Public Hospitals Authority Managing Director Aubynette Rolle has acknowledged the complaint and initiated an internal review process. Meanwhile, Hall continues her hospitalization while battling multiple sickle cell complications that previously required transfer from Rand Memorial Hospital in August.
The case underscores the critical intersection of healthcare staffing shortages, institutional accountability, and patient rights, raising fundamental questions about systemic safeguards for vulnerable patients during non-visiting hours.