The Association of Economists in Suriname (VES) has unveiled an ambitious proposal to transform Wanica Hospital into a specialized center dedicated to treating chronic diseases including diabetes, cardiovascular conditions, and chronic kidney diseases. This strategic initiative aims to address the growing healthcare demands within Suriname’s fastest-growing district through an integrated care model that promises enhanced efficiency, affordability, and sustainability.
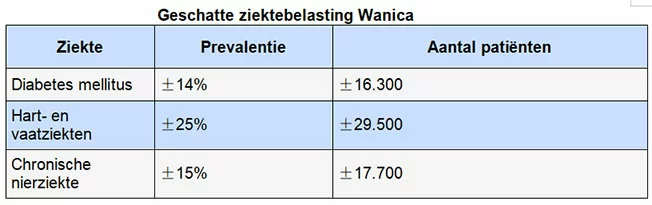
With approximately 118,000 residents, Wanica represents a critical demographic shift in Suriname’s population landscape. The district’s substantial proportion of inhabitants aged 40-70 years creates heightened vulnerability to chronic health conditions. According to VES data, diabetes affects approximately 14% of the population (16,300 individuals), cardiovascular diseases impact 25% (29,500 individuals), and chronic kidney diseases affect 15% (17,700 individuals). Collectively, these conditions represent over 60,000 patients, many experiencing multiple comorbid health challenges.
The proposed healthcare revolution centers on implementing ‘care pathways’ – integrated treatment trajectories that consolidate prevention, diagnosis, treatment, and aftercare services according to specific disease profiles. This innovative approach would establish dedicated diabetes care pathways, cardiovascular care pathways, and renal care pathways within Wanica Hospital.
Economic analysis indicates that care consolidation would significantly reduce duplicate testing, optimize staff utilization, and minimize medication waste. These efficiencies would enable the hospital to treat more patients while maintaining lower structural operational costs.
Financial projections estimate annual operational costs for the proposed care pathways at approximately USD 16 million, against expected annual revenue of USD 19-20 million. The resulting 10% profit margin is conceptualized not as profit maximization but as essential capital for maintenance, innovation, and improved staff compensation.
A mixed financing model proposes 30% government funding, 30% through employee and employer premiums (including SZF reform), and 40% private investment. With phased implementation over four to five years, the hospital could achieve break-even operation within six to seven years.
The specialization initiative is expected to generate substantial employment opportunities for nurses, laboratory technicians, dialysis specialists, dietitians, data analysts, and healthcare managers. Increased productivity would create financial flexibility for competitive salaries, potentially reducing the emigration of healthcare professionals abroad.
VES envisions Wanica Hospital as the central hub within a national healthcare network, connecting with RGD clinics, regional hospitals, and telemedicine facilities serving interior regions. This model demonstrates how demographic realities, economic considerations, and policy vision can converge to create structural healthcare reform with nationwide implications.